Background
Osteosarcoma is a malignant bone tumour that originates from primitive bone-forming mesenchymal cells.1 It is the most common primary bone cancer in children, adolescents, and young adults, with a peak incidence in the second decade of life.1,2 It has a male predominance and usually affects the metaphyseal regions of long bones, especially around the knee.1,3 The etiology of osteosarcoma is unclear, but some risk factors include previous irradiation, Paget’s disease, polyostotic fibrous dysplasia, benign bone tumors, and genetic syndromes such as hereditary retinoblastoma and Li-Fraumeni syndrome.1,4–6
Osteosarcoma patients typically present with localized pain and swelling that may be related to strain, trauma, or infection.2,3 The pain may be nocturnal or persistent and may interfere with joint movement.4 Radiological features of osteosarcoma include increased intramedullary sclerosis with permeative destruction, elevation of periosteum resulting in Codman’s triangle or sunburst appearance, and new bone formation in soft tissues.4,7,8 Osteosarcoma can be classified into different subtypes based on the location within the bone (central, parosteal, periosteal), the degree of differentiation (conventional, telangiectatic), and the histological variation (osteoblastic, chondroblastic, fibroblastic).9–11
Osteosarcoma has an incidence rate of 4 to 5 per million persons per year in children and adolescents.11,12 However, this rare disease is often misdiagnosed or diagnosed late, especially in low-resource settings. In sub-Saharan Africa, osteosarcoma poses a significant challenge for the health system, as it requires specialized care and multidisciplinary management.11,12 The epidemiology of osteosarcoma in this region is poorly understood, as there is a lack of reliable data from population-based cancer registries.
According to the Global Burden of Disease report, osteosarcoma was responsible for 0.1% of all cancer deaths and 0.2% of all cancer disability-adjusted life years (DALYs) in sub-Saharan Africa in 2019.13 However, these estimates may not reflect the true burden of the disease, as they are based on modelling and extrapolation from other regions. Therefore, there is an urgent need for more research and investment in data production, analysis, and interpretation to inform national cancer policies and programs in sub-Saharan Africa.
One of the factors that contributes to the poor outcomes of osteosarcoma patients in sub-Saharan Africa is the late presentation of the disease.14,15 Muthupei and Mariba reported a 5-year survival rate of 7.5% in their 2000 study of 66 osteosarcoma patients at a tertiary hospital in South Africa (SA), which is comparable to outcomes from the 1950s in developed countries.14 In 2010, Shipley and Beukes reported on 30 patients with osteosarcoma treated at another SA tertiary institution.16 Half of their patients presented with metastases.5,16 The majority of patients in these studies from developing countries presented with advanced disease, to which the authors attributed their poor outcomes compared with the far better survival rates in developed countries .5,16 Marko et al observed that patients in countries with medium/low Human Development Index had longer delays and higher prevalence of metastasis at diagnosis compared to those in countries with very high/high Human Development Index.17 Noor et al. had similar findings in a study in Cambodia, with a 5-year survival rate of only 8%, citing late presentation and cultural preferences as the main factors responsible for the poor outcomes.5,18 In summary, the factors contributing to diagnostic delay may be related to the patient (lack of knowledge around bone tumours, limited finances to travel to a health care facility,lack of finances to pay for diagnostic tests), the provider (limited diagnostic capacity, unavailability of in house specialists), or the country (no well-established referral systems, failure to supply stocks or service diagnostic tools e.g. magnetic resonance imaging).5,19
These studies highlight the need for early detection and referral of osteosarcoma cases, as well as improved access to quality care and supportive services for patients and their families.
The treatment of osteosarcoma has improved significantly in the last 25 years, especially for patients with localized disease.1,2,7,14 This is attributed to the advancement in multimodal therapy that combines surgery and chemotherapy.3,5,15,20 Several randomized trials have shown that the combination of neoadjuvant and adjuvant chemotherapy with surgery significantly improves the cure rates and reduces the local and distant relapse rates.21 The surgical options include limb salvage or amputation depending on the tumor location, size, extent, and response to chemotherapy.7 The goal of surgery is to achieve adequate local control and preserve function.7
Therefore, this study aimed to describe the clinical features, diagnostic methods, and treatment modalities associated with osteosarcoma in Malawi. The study also investigated timelines between symptom onset, healthcare consultation, diagnosis, treatment, and outcome. To our knowledge, this is the first study to address this topic in this setting.
Methods
We conducted a retrospective review of medical records of 25 patients who were diagnosed with osteosarcoma at Queen Elizabeth Tertiary Hospital between January 2011 and December 2016. Queen Elizabeth Tertiary Hospital is the largest referral center for oncology patients in Malawi. We obtained an approval to carry out the study from the College of Medicine Research and Ethics Center (COMREC) (P.02/18/2364. Formal request was written to head of department in Oncology Unit, Surgery Department and hospital director to have access to patients’ charts. No informed consent was obtained from the patients since the study did not involve intervention on patients or contacting the patients.
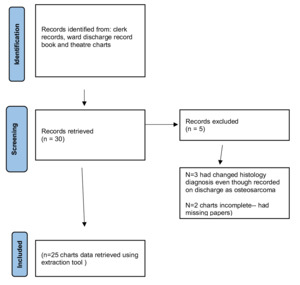
We included all inpatients who had been diagnosed with osteosarcoma during this period based on histological or radiological criteria. We excluded patients who had insufficient data or whose diagnosis changed to another malignancy after review of histology. Refer to chart 1 delineating inclusion criteria.
We collected data on patient demographics, presenting symptoms, diagnostic procedures, histological findings, treatment options, and time intervals from symptom onset to treatment initiation using a data collection sheet.
We defined symptom onset as the date when the patient first noticed any symptom related to osteosarcoma; presentation as the date when the patient first visited low level health care system and from low level care to first visit at tertiary hospital; diagnosis as the date when histological or radiological confirmation was obtained; treatment as the date when any therapeutic intervention was started; patient delay as the time interval from symptom onset to presentation; professional delay as the time interval from presentation to diagnosis; system delay as the time interval from diagnosis to treatment; and total delay as the time interval from symptom onset to treatment.
We used Excel software (Microsoft Corporation, Redmond, WA) to build our database and generate tables and charts. We used IBM SPSS Version 1.0.0-1762 (1.0.0-1762) to perform descriptive statistics and frequency analysis.
RESULTS
The study examined the epidemiology, diagnosis, and treatment of osteosarcoma cases at Queen Elizabeth Tertiary Hospital in Malawi.
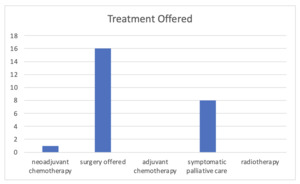
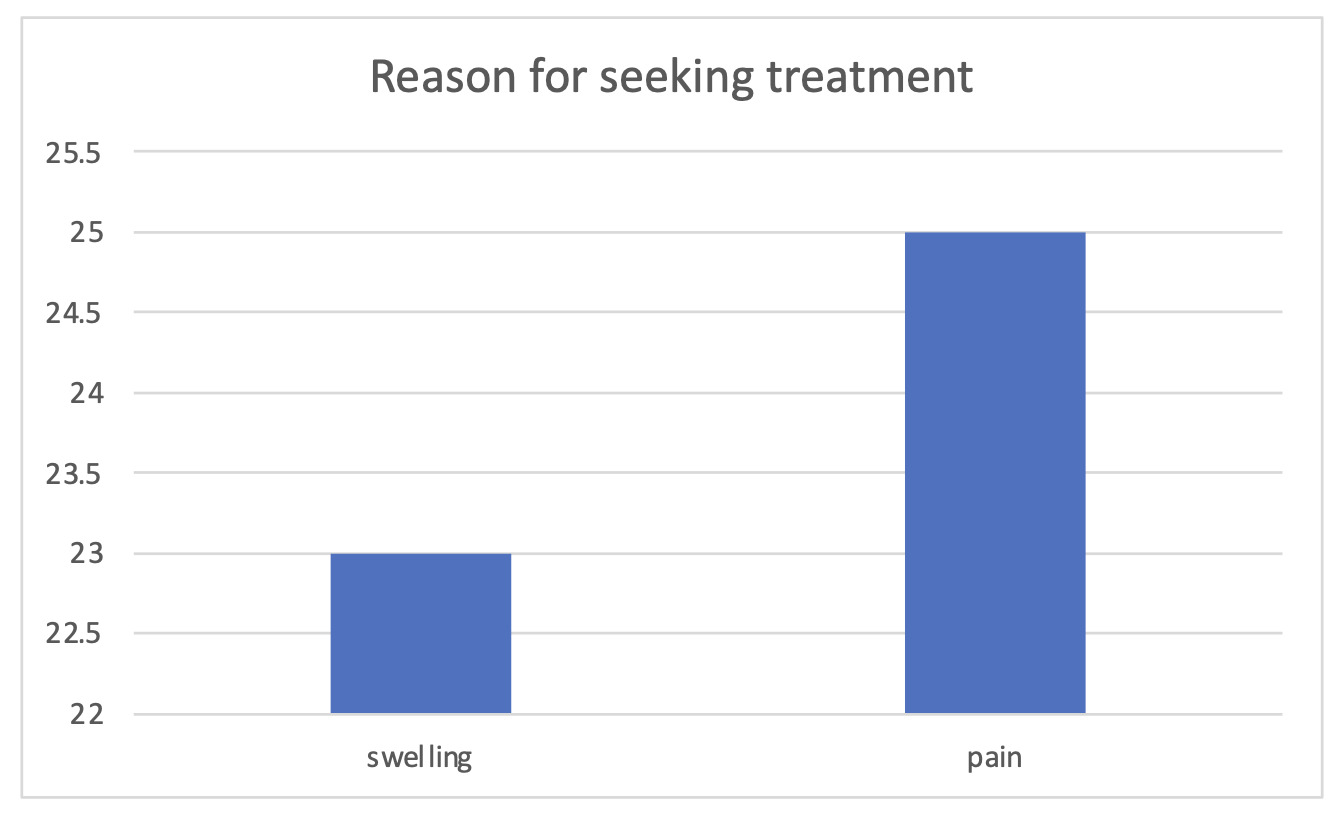
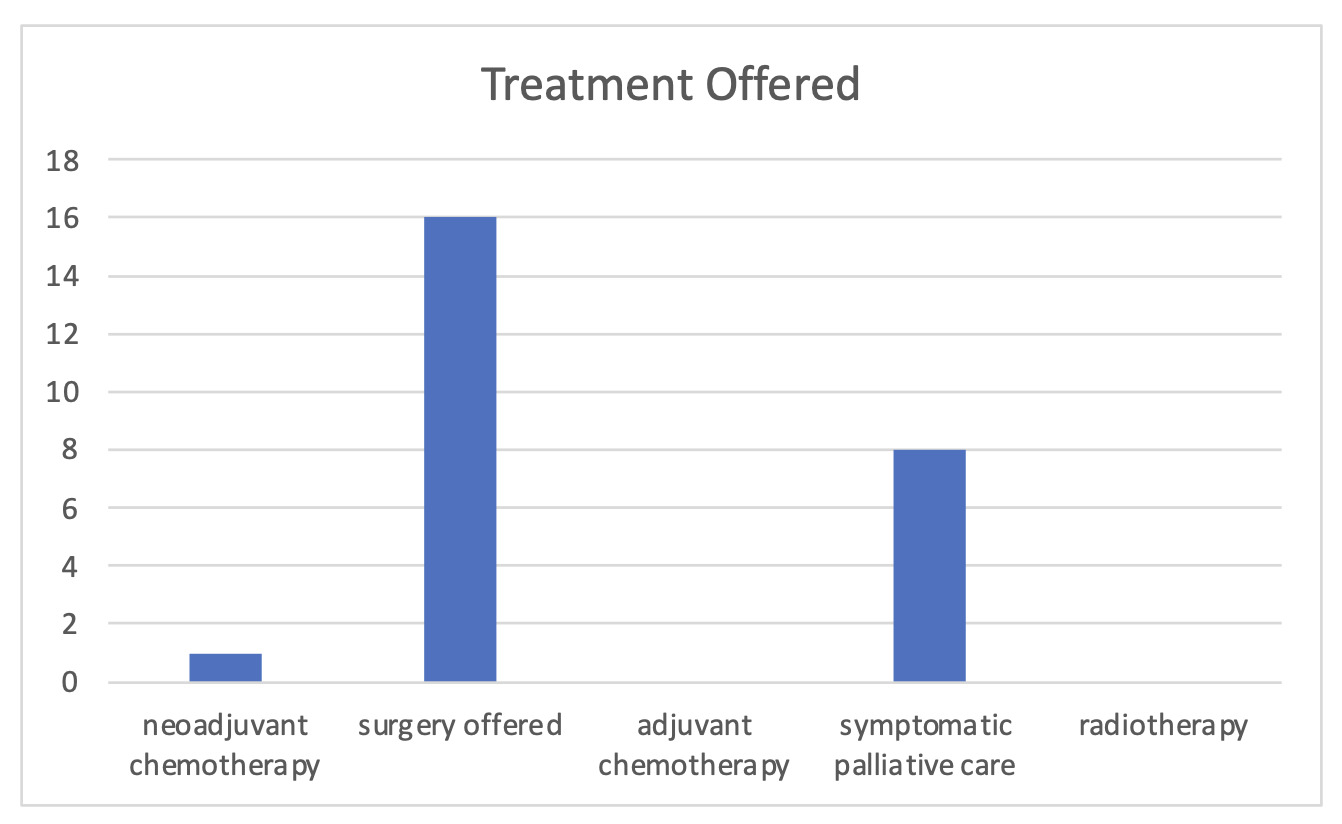
The main findings were: Osteosarcoma was a rare malignancy, accounting for only 0.22% (n=25 out of 11,165) of all cancers registered during the study period.22 The patients had a median age of 25.04 years (Standard Deviation (SD) =11), with an equal sex distribution (13 males and 12 females) and a wide age range (13-58 years). The most common symptoms were pain 100%(n=25) and swelling 92% (n=23) refer to figure 1, and the most common site was the knee refer to figure 4. The common site of osteosarcoma was around the knee 44% (n=11) refer to diagram 1. The diagnosis was confirmed by histology in 56%(n=14) of cases and by radiography in 44% (n=11) of cases. 76% (n=19) had incisional biopsy done but only 56%(n=14) received histology results. No tumor grade was recorded in any histology report. Except for 16%(n=4) cases that presented with metastasis, which is stage 3 on Enneking classification, the rest could not be assigned an Enneking stage. The median duration from symptom onset to presentation at the tertiary hospital was 8.5 months, indicating a long delay in seeking care. The mean time from diagnosis to treatment was 16.4 days. The treatment offered (figure 2 and 3) included amputation in 48% (n=12) of cases, symptomatic palliative care in 32%(n=8), limb salvage surgery for 4% (n=1) of the cases, and neoadjuvant chemotherapy only 4% (n=1). No patient received adjuvant chemotherapy. 12% (n=3) of our patients declined to have an amputation.
The study did not report on the survival or outcome of the patients due to lack of digitized data for outpatient care or cancer registry that actively followed up patients in outpatient setting. This resulted in the loss of the information to determine survival or outcome of the chosen treatments.
Table 1, summarizes the demographic, clinical, diagnostic, and treatment characteristics of the study population.
DISCUSSION
Osteosarcoma is a challenging disease to diagnose and treat in Malawi due to its rarity, nonspecific symptoms, lack of histological grading and staging, limited treatment options , and long delays in the care pathway . Our study provides some insights into these issues based on a retrospective review of medical records of 25 osteosarcoma patients at Queen Elizabeth Tertiary Hospital.
Our study population had a median age of 26 years , which is higher than the peak incidence age reported in other studies .1,3,4 This may reflect a different epidemiology of osteosarcoma in Malawi or a selection bias due to late presentation or referral. We also found an equal sex distribution among our patients , whereas other studies have reported a male predominance .23–25 These findings suggest that there may be some demographic differences between osteosarcoma patients in Malawi and those in other settings, but sample size was small to make definitive conclusion.
The most common presenting symptoms in our study were pain and swelling , which are consistent with previous reports .7,9,26,27 However ,the median duration of symptom onset to presentation at tertiary hospital for osteosarcoma patients in Malawi was 8.5 months, which is much longer than what has been reported elsewhere.2,8,23,26,28 For example, a study from Ethiopia reported a median duration of 3.5 months for bone sarcoma patients,8 while a study from Nigeria reported a mean duration of 36 months+/-4.1 months for osteosarcoma patients,27 Tanzania sarcoma study by Siwillis et al.28 had reported duration of 5 months.In contrast, studies from developed countries have reported much shorter durations, such as 1.2 months in the UK,21.3 months in the USA,23 and 1.5 months in Canada.26 These differences may reflect the variations in the availability and accessibility of health care services, the awareness and knowledge of osteosarcoma symptoms, and the socio-economic and cultural factors that influence health-seeking behavior among osteosarcoma patients in different settings.
Unfortunately, we could not obtain data on symptom onset to first visit at any health center because it was not documented in the files, which would have helped us to better understand this aspect.
The confirmation of osteosarcoma diagnosis by histology in only 56% of the cases in Malawi is lower than the rates reported in other African countries, such as Ethiopia (86.4%), Tanzania (100%), and South Africa (100%).8,9,28 This suggests that there is a need to improve the availability and accessibility of biopsy services and histopathology laboratories in Malawi.The lack of tumor grade or staging in the Malawian study is also a major limitation, as these factors are important for prognostication and treatment planning. In contrast, other studies from Africa and elsewhere have reported the tumor grade and stage of osteosarcoma patients. The absence of standardized reporting or quality control for osteosarcoma diagnosis in Malawi may affect the accuracy and outcomes of these patients. The use of radiography as the sole diagnostic method in 44% (n=11) of the cases in our study is not recommended, as radiography alone cannot differentiate between benign and malignant bone lesions. Moreover, radiography cannot provide information on the histological subtype, and grade of osteosarcoma, which are essential for determining the appropriate treatment regimen. Therefore, radiography should be used as an adjunct to biopsy and histopathology, not as a substitute.
The common site of osteosarcoma was around the knee 44% (n=11) refer to diagrammatic presentation. This is in keeping with studies done in other centres.1,2,28
The mean time from diagnosis to treatment was 16.4 days in our study , which is comparable to what has been reported in other low- and middle-income countries.15,19,29However , we found that only 4% (n=1) of our patients received neoadjuvant chemotherapy , which is considered as an essential component of multimodal therapy for osteosarcoma .4,19,21This was likely be due to lack of resources , expertise , protocols , or compliance for administering chemotherapy in Malawi,during the period data was collected. Furthermore, we found that only 4% (n=1) of our patients underwent limb salvage surgery, whereas 48%(n=12) underwent amputation. This may be due to lack of facilities, equipment, skills, or prosthesis for performing limb salvage surgery in Malawi. Limb salvage surgery has been shown to improve function and quality of life without compromising survival compared to amputation.16,30
However, some patients may refuse limb salvage surgery due to fear of recurrence or preference for amputation. We found that 12%(n=3) of our patients declined amputation, which may be due to cultural or religious reasons, lack of social support, or poor understanding of the disease and its treatment.
The comparison of survival rates between our study and other studies is difficult, as the QECH study did not report the follow-up duration or the number of deaths among the patients. However, based on the available data, it can be inferred that the survival rate of osteosarcoma patients in Malawi is likely to be low, as 52% (n=13) of them presented with advanced disease (16%(n=4) with metastasis to lung and liver and 36%(n=9) with unspecified advanced disease at diagnosis), which is associated with poor prognosis.16,28,31 In addition, most of them did not receive adequate treatment, such as chemotherapy, radiotherapy or surgery, due to various reasons, such as late referral, or refusal. These factors may also contribute to the low survival rate of osteosarcoma patients in Malawi. In comparison, other studies from Africa and elsewhere have reported higher survival rates for osteosarcoma patients who received multimodal treatment, such as chemotherapy, surgery, and radiotherapy.16,19,30
Our study has some limitations that should be acknowledged. First, it was a retrospective study based on medical records that may have been incomplete or inaccurate. Second, it was conducted at a single tertiary hospital that may not be representative of the whole country. Third, it had a small sample size that may limit the generalizability. Fourth, it did not include data on survival or recurrence rates, which are important indicators of prognosis and quality of care.
Despite these limitations, our study provides some valuable information on the clinical features, diagnostic methods, treatment modalities, and time intervals of osteosarcoma patients in Malawi. It also highlights the challenges and gaps in the diagnosis and management of this disease in this setting. There is a need for increased awareness and suspicion among primary health care providers, improved access to diagnostic facilities and specialized care, and multidisciplinary collaboration to optimize the management and prognosis of osteosarcoma patients in Malawi.