Introduction
Background
Since the description of surgery as a ‘forgotten stepchild of global health’, the support for surgical considerations in health systems’ strengthening, and global health improvement have increased.1,2
The Sustainable Development Goals instruct that improving essential and emergency surgical care are rights of global citizens, which will improve health and health equity.3 These were ratified by the World Health Assembly Resolution 68.15; that made accessing quality and timely ‘Emergency and Essential Surgical Care and Anaesthesia’, a component of the Universal Health Coverage.3,4 In 2015, the Lancet commission suggested the measuring of access to timely surgery (the population accessing surgery within 2 hours) as one of six metrics, determining the capacity of health systems to provide safe surgical care.2,5
The availability of healthcare services and health-seeking behaviours broadly determine access to healthcare.6,7 The geospatial access to health services is evaluated based on accessibility (proximity to healthcare services) and availability (spectrum of health services and their supply); while being measured using time-to-hospital, population’s demand for services and hospitals’ capacity.8 Whilst there exist significant individual influences to health-seeking behaviours,9 the utilization of health facilities and healthcare givers depend on proximity, affordability, ease-of-access, potentially good treatment outcomes and kind personnel.2,6,7,9 Specifically, evaluation of access to surgery is based on timeliness, surgical care capacity, the safety of the patient, and the ability to pay for care.5
Rationale
Thirty percent of the global disease burden is surgical,5 and prompt surgical care potentially reduces the morbidity and mortality (estimated at 16.9 million people globally, in 2010) associated with surgical emergencies.2,9–11 Several emergency room (ER) visits require urgent surgical intervention and emergency surgical procedures.12 Trauma (road traffic crashes and firearms injuries) is a leading cause of ER visits in America.13,14 Some West African series reported trauma-related ER mortality to be between 30% and 70%.15–17
Access to safe and affordable surgery is considered to be inadequate,18 as about five billion people are without access to essential surgical procedures globally2,5,18,19; this is worse in low- and middle-income countries.19,20 The above access to surgery indices is despite 312 million surgical procedures which are performed annually, globally.2,18 Thirty-five percent of the global population are resource limited, yet only 3.5%5 to 6% of global surgical procedures are done in poor climes,18 rural or peri-urban areas.2,19 Sub-Saharan Africa’s surgical burden ranges between 257.8 - 294.7 million people18 and estimated at 38 DALYS (Disability Adjusted Life Years).21
There is a paucity of studies in the literature on the determinants of access to emergency surgical care in Nigeria. This study was therefore conducted, to provide a data base of access to acute and emergency surgical care for the formulation of evidence-based healthcare services policies.
Objectives
We established the perspectives of resident doctors to the dynamics of access to emergency surgeries at the University College Hospital, Ibadan, Nigeria. This was accomplished by interrogating the patient-related, healthcare giver-related and health-institution related domains.
Methods
The study ran between September 2020 and January 2021, at the University College Hospital Ibadan. It was a cross-sectional study of resident doctors involved in the care of patients who presented with surgical emergencies.
The participants were resident doctors from the following departments: surgery, plastic surgery, neurosurgery, orthopaedics, otorhinolaryngology, ophthalmology, obstetrics and gynaecology, oral and maxillofacial surgery, anaesthesia as well as the ER. Resident doctors were chosen because they are usually the first-on-call, hence have a practical knowledge of the prevailing circumstances surrounding emergency care.
We did a systematic random sampling of the resident doctors in the purposively selected departments (equally weighted) above. After obtaining a sampling frame, the resident doctors were arranged alphabetically and assigned numbers. Numbers were selected from a-priori selection criteria, where random numbers were generated from a table of random numbers until the sample size was reached. All the doctors representing the numbers were contacted and those who gave consent were recruited as participants.
The sample size was estimated using STATA/MP 15.0 (Stata Corp, college station, TX), using the command [power r-squared 0.5, alpha (0.001) power (0.9) ntested10] for a multiple linear regression statistic with the following parameters. Significance level set at 0.001, power set at 90%, testing for possible ten covariates and an assumed effect size of R-squared of 0.5. A minimum sample size of 51 participants was determined.
The outcome measures were reported as delay factors for the patient-related, healthcare-giver related and the health institution-related domains (ordinal scale).
All the participants completed electronic, pre-tested, four-sectioned, 57-item, structured, self-administered questionnaires in English language. The questionnaires were built using results from a systematic review on the research queries and pre-tested on 10 resident doctors from a different setting, prior to it being reviewed to the final version. The initiation with progression through to the submission of the study instrument was recorded as consent for the study. We de-identified the biodata and professional data, and the Likert-scale-styled sections on patient-related factors, healthcare-giver related, and health institution-related determinants of access to emergency surgery formed the database of the study. The content validity of this instrument was assessed by 5 clinical researchers, who were independent of the study investigators. The item-level and scale-level (based on the average and universal agreement methods) content validity indices were all 0.93, and satisfactory.
The data were obtained using Google forms (Microsoft Corp., Redmond, WA) to generate a Microsoft Excel (Microsoft Corp., Redmond, WA) spreadsheet, in-view of the COVID-19 pandemic. Analyses for summary statistics (means, standard deviations, proportions) were done. The Likert-scale-styled responses were trichotomized, into positive, negative, and neutral responses and analyzed as proportions.
We obtained ethical approval (UI/EC/20/0318) from the University of Ibadan/University College Hospital (UI/UCH) Health Ethical Review Committee and prospectively registered the study protocol in ClinicalTrials.gov (NCT04487496).
This study only reflected the perspetives of the respondents, who were resident doctors, and they created responses as they adjudged could possibly affect other colleagues, as well as the patients and the health institution.
Results
Demographics and clinical specialties of the respondents
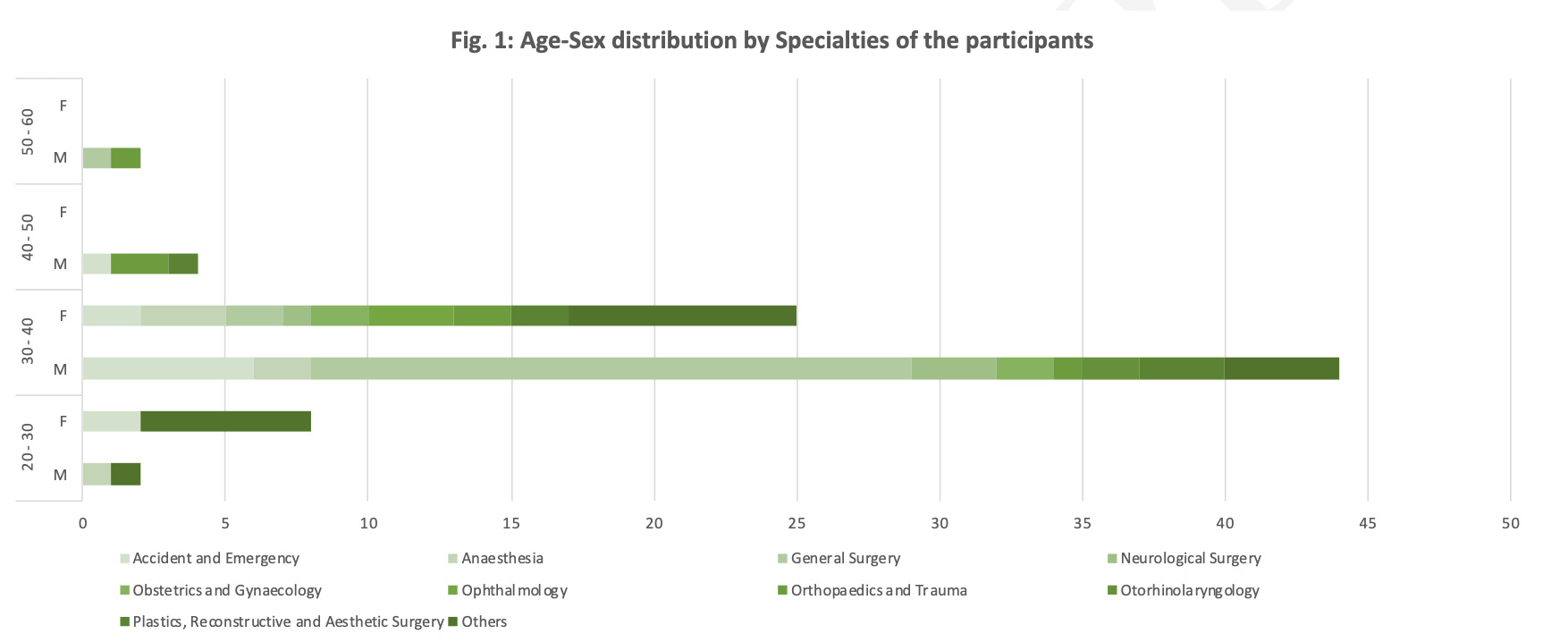
Eighty-five participants completed this study. Fifty-three (62.4%) were males. The modal age group [69 (81.2%)] was 30 - 40 years, and the average age was 34.4±5.22 years (mean ± standard deviation). The participants had spent an average of 8.7±5.08 years post-medical degree, and an average of 4.1±3.85 years in their specialty. General surgery residents were the modal resident-doctor category, accounting for 23(27%) participants, while the emergency room doctors were 11 (13%) participants. The other demography data are shown in Figure 1.
Determinants of access to emergency surgery
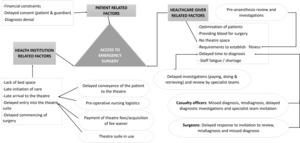
A theoretical framework schema, showing the synopsis of the determinants of access to surgery from this study is presented in Figure 2. It presents the interaction of the determinants with the patient-related, healthcare-giver related and health institution-related dynamics.
The reported major patient-related determinants of access to emergency surgery were from lack of funds (83/97.7%), delayed patient consent (68/ 80.0%) or guardian consent (63/ 74.1%) and delays in accepting diagnosis (60/ 70.6%). The superstitious belief of patients (59/ 69.4%) generating aversion for surgery, other patients’ spiritual belief (47/ 55.30%) and the requirement to get an assent from a spiritual leader (36/ 42.4%) were other patient-related dynamics and are presented in Figure 3.
Clinical and non-clinical personnel contribute to emergency surgical services delivery. Anaesthesiologists (66.0%) were the doctor category most likely to cause delayed access to emergency surgical procedures; with casualty officers (21.0%) and surgeons (13.0%) being less significant causes. Surgeons (61.0%) were reported to reduce delays most likely, with Anaesthesiologists (26.0%) and casualty officers (13.0%) making much smaller contributions.
Healthcare givers were perceived to modify access to emergency surgery, during the acquisition of blood for surgery (72/ 84.7%), optimization of patients for surgery (72/ 84.7%), with the lack of access to theatre space for surgery (71/ 83.6%) and delays in fulfilling the requirements for establishing fitness for surgery ( 61/ 71.8%) amongst other factors presented in Table 1.
The diagnosis of surgical emergencies was delayed mostly during the performance of diagnostic investigations (82/ 96.5%). These include paying for the investigations (82/ 96.5%), the laboratory performing the investigations (75/ 88.2%) and the retrieval of results (63/ 74.1%). Other diagnostic delays were from late reviews by the specialty team (68/ 80.0%) and late reviews by senior members of the specialty team (64/ 75.3%).
Casualty officers and/ or primary care physicians affect access to emergency surgeries mostly from missed diagnosis (72/ 89.7%) and misdiagnosis (71/ 83.5%), but also while optimizing patients (56/ 65.9%), ordering diagnostic investigations (54/ 63.5%) and referring patients to the surgical team (49/ 57.7%). Others are presented in Table 1.
Anaesthesiologists affect access to emergency surgery by them being fatigued (75/ 88.2%) or experiencing staff shortage (76/ 89.4%); also during delays from the investigations ordered by the anaesthesiologists (76/ 89.4%) and from the pre-anaesthesia review (70/ 82.4%).
Surgeons alter access to emergency surgery mostly from shortage of surgeons (71/ 83.5%); the optimization of patients for surgery (57/ 67.1%), surgeon fatigue (54/ 63.5%) and delayed response to surgical consult (54/ 63.5%); others are presented in Table 1.
The health-institution related dynamics of access to emergency surgery included, limitations in accepting patients due to lack of bed space (70/ 80.4%), delays in entering the theatre suite (64/ 75.3%) and in the processing of payment for surgery or receipt of fee-waivers (74/ 87.1%) amongst others as detailed in table 2. The processes for moving the patient to the theatre were delayed by pre-operative nursing logistics (55/ 64.7%), from the theatre trolley picking up the patient from the ward (60/ 70.6%) and from the theatre suites being in use (64/ 75.3%).
Discussion
Determinants of access to emergency surgery
A schematic representation of the studied domains and their major determinants are summarized in Figure 2 above. The following subsections will give more details of these roles as reported by the participants.
The time intervals, as well as the events therein, that occurred from symptom onset, through to the utilization of health services had been studied. The findings evolved, with attempts to proffer precision and are presented below.
Safer’s22,23 patient-delays three-stage model, was described from observation of symptoms to actual care-seeking. These were the appraisal delay – periods of symptom evaluation and acceptance as indicative of illness, illness delay – initial symptom onset to time of decision for appropriate care. The utilization delay – is from decision to seek care to when a healthcare-giver is sought.22,23
Andersen’s model included the stages of appraisal, illness, behavioural, scheduling, and treatment.22,24 They posited that describing the intervals between the delays was better. They expanded Safer’s ‘utilization delay’ stage into three. The behavioural delay – described from when an illness is adjudged to require medical care to when the decision to act is made. The scheduling delay defines from the decision to act to when a healthcare giver is seen. The treatment delay describes the period between first seeing a healthcare giver and commencing treatment.22,24
Walter and colleagues proposed a four-stage Model of pathways to treatment, after analysing Andersen’s model. They stated that appraisal interval occurs between patient’s detection of body changes and the need to see a healthcare-giver. The Help-seeking interval occurs following the appraisal interval to the first visit to a healthcare-giver. The Diagnostic interval occurs after the health-seeking interval until diagnosis is concluded. The pre-treatment interval ends at the commencement of treatment.22
The Lancet Commission on Global Surgery (LCoGS) recommends the ‘Three Delays Framework’.25 The First delay is from geographic constraints, poverty, cultural belief, low-level health literacy, poor awareness of health services availability or low confidence in their services.25 The Second Delay is from scarce health facilities, long travel-times, and travel distance, as well as poor public infrastructure and ambulance services.25 The Third delay occurs from shortages in skilled personnel and medicines and poor infrastructure (electricity, water, and oxygen).25
Patient-related determinants of access to emergency surgery
The major patient-related factors were financial constraints, delays in the patient or guardians giving consent for surgery and delays in accepting the diagnosis. Spiritual or behavioural patient-related delays existed, with aversions for surgical procedures emanating from superstitious and spiritual ideations as well as requirements for ratification by a spiritual leader.
Okeke et al26 reported that delayed starting of elective surgeries were mostly caused by patients; including poor finances (affecting 9-25% of delays), delays in giving consent and in the provision of blood for surgery.26
Poorer people travel longer distances to reach facilities able to provide emergency surgery.8 People in the lower socioeconomic class, used poorer performing facilities according to de Jager.27 We postulate that poor patients may indirectly be averse to surgical procedures (for fear of the inability to afford them), thus creating a pseudo-denial of the surgical diagnosis and possibly delays in giving consent for surgical procedures. Some patients could also declare false financial constraints in the setting of superstitious fear of surgeries and/or while waiting to get permission from a spiritual leader to proceed with surgical procedures.
A potentially significant confounder for the patient-related access determinants could be the fact that some patients who have surgical emergencies may have lost their capacity to make decisions and/or act on the decisions by themselves. These may be either direct or indirect consequences of the illness process. Thus, even though the patient may have come to seek ‘health-help’, or has been brought by care-givers (supposedly removing the chances of delays prior to the scheduling stage). By virtue of the patients or their legal representatives retaining the capacity to not accept emergency-surgery-requiring diagnoses (as reported by our respondents), the suggestion of a potential down-staging of the decision making process is evident, since the capacity to decide to act on the diagnosis is invariably lost as well.
Healthcare-giver related determinants of access to emergency surgery
Health facility workers are not all healthcare givers. Generally, we categorized them as clinical and non-clinical, based on the contact or lack of contact with patients. They have the potential to alter in-hospital access to surgical procedures.The participants identified differential roles of medical specialists in modifying access to emergency surgery. They agreed that anaesthesiologists (who constituted 30% of the participants) more likely caused delays than casualty officers and surgeons. This was reversed for those likely to reduce delays, as surgeons were the choice. Okeke et al26 had reported a discordant finding with the surgeon factor (28.5%) was a more significant cause than the anaesthetic factor (4.5%). Casualty officers were shown to modify access mostly from missed diagnosis, misdiagnosis, delays in optimizing patients for surgery, in ordering diagnostic investigations and in referring to surgical teams.
The participants identified that healthcare-givers’ mostly modify access from ensuring the patients’ fitness for surgery, optimization of patients’ clinical and laboratory parameters, acquisition of blood, and the absence of theatre space amongst others.
The healthcare-givers determine the decision to accept a patient for care, based on objective (absence of facility to care for patients) and subjective (staff fatigue, shortage, unavailability, e.t.c) parameters. The doctor-to-patient ratio is thus a significant player here and even more so, the specialist-to-patient ratio.
Diagnosing surgical emergencies was significantly delayed by diagnostic investigations and the surrounding events. These were paying for the investigations, performing the investigations and obtaining the results of investigation . Doctors cause diagnostic delays by delaying reviews by the specialty team.
Kajja et al28 reported the unavailability of blood for surgery as the second leading cause of delayed starting of elective surgery. This delay was higher for each additional unit of blood ordered for peri-operative use.28
Health institution-related determinants of access to emergency surgery
Institutional mediators of access to emergency surgeries were reported by Caesar and colleagues as major causes of delayed commencement of emergency orthopaedics procedures.29 The absence of bedspace, delays in entering the theatre suite and payment for surgeries or receipt of theatre fee-waivers, were shown by our participants to be related to the health facilities. The delays in entering the theatre suite, were shown to be caused by prolonged pre-operative nursing logistics, delays in theatre trolley picking the patient and the theatre suites being in use.
These factors are related to health facility access challenges. It is clichéd that the access metrics of staff, stuff, space, and systems are still limited for surgical care delivery in Sub-Saharan Africa, as 90% of the sub-Saharan African residents have access to one operating theatre per 100,000 persons.5 Smaller capacity hospitals more commonly have adverse surgical events; supporting the fact that the number of beds in a hospital influences the quality of care provided.21 The urban-poor have higher risks of post-operative adverse events, with those in the lower socioeconomic class being served by lower performing health facilities.27 Specifically, the shortage of theatre space was reported by Kajja et al28 as the leading cause of delayed commencement of elective surgeries, in concert with our finding. Caesar et al29 had shown that the varied shortages in hospitals are causes of delays, in keeping with our finding of staff shortage as a cause of delay.
Rural minorities in California, have more access disparities (longer travel times, and spatial access to emergency surgical services were about 20% of the average for the State’s access metrics).8 Though these minorities had higher demand for the emergency general surgical services, they had inadequate services.8
This study only reflected the perspetives of the respondents, who were resident doctors, and they created responses as they adjudged could possibly affect other colleagues, as well as the patients and the health institution. The distribution of the participants was skewed towards the surgeons, who had more specialties and thus, invariably had much more contributions. More quantitative efforts to investigate this theme would be necessary.
Conclusion
In-hospital access to emergency surgery metrics is modified by clinical and non-clinical members of the hospital staff, mostly by altering delays in diagnosis, pre-operative optimization of patients, conveyance of patients to the theatre, and the surgical procedure itself. In-hospital delays from patients and/or their caregivers are from poor finances, diagnosis denial and delayed giving of consent. Health facility’s contributions come from delays in accepting patients for care (on account of saturation of the hospital’s bedspace) and entry into the theatre complex as well as the theatre suite itself. Payment related causes of delays were noted amongst all three studied domains.
Arising from these findings,we suggest policy drifts towards the provision of physician-run ER point-of-care diagnostics, as well as increased ER bed-space capacity and the rates of transfer of patients to the in-patient services. We desire the expansion of the health insurance coverage, thus reducing out-of-pocket payments, while expanding the size of surgical and anaesthesiological manpower.